Key Takeaways
- Cystic acne is the deepest, most painful form of acne.
- Hormones, genes, and stress work together to set off flare‑ups.
- Dermatologists‑only medicines—like isotretinoin and cortisone shots—often do the heavy lifting.
- Food does not cause cystic acne,
- You can lower the risk of new cysts by spotting warning signs quickly,
What Makes Cystic Acne Different?
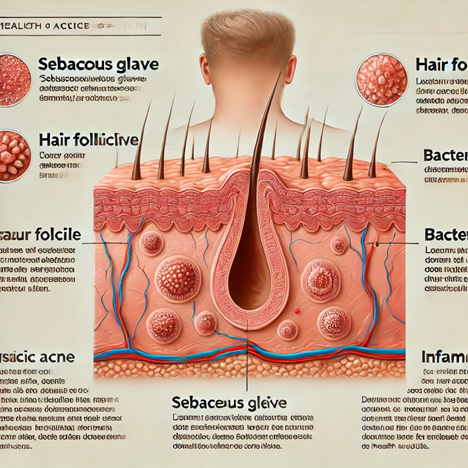
Cystic acne is not “just a big pimple.” It is a swollen pocket deep inside a hair follicle that fills with oil, dead skin, and bacteria. Because the cyst sits so low, normal cleansers and spot creams can’t reach it. That is why it hurts more and hangs around longer than whiteheads or blackheads.
I first saw the difference during medical school. A classmate’s “pimple” grew into a red knot the size of a pea by noon. By evening, the cheek was tight and throbbing. A faculty dermatologist lanced it, and thick fluid emerged from far beneath the surface. That picture has stayed in my mind whenever a patient says, “It’s just one bump.”
Cysts form where oil glands are densest—the jawline, neck, back, and shoulders. They erupt in waves that can stretch over months or even years. Unlike milder acne, cysts almost always leave marks if squeezed or ignored. Understanding this depth is the first step toward smart treatment choices.
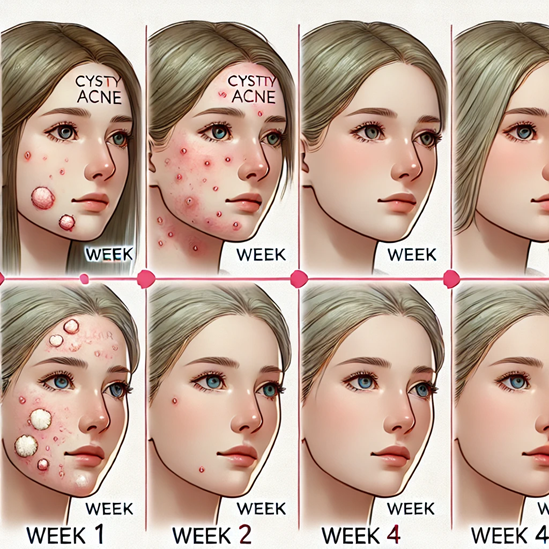
Spotting the Signs Early: Recognizing Cystic Acne
Cysts often start as a tender spot you can feel before you see anything. It may itch or ache when you smile. Within 24 hours it swells, and the skin looks stretched and shiny. There is rarely a white “head,” so squeezing does nothing but deepen the injury. My rule in the clinic: If it hurts before it shows, suspect a cyst.
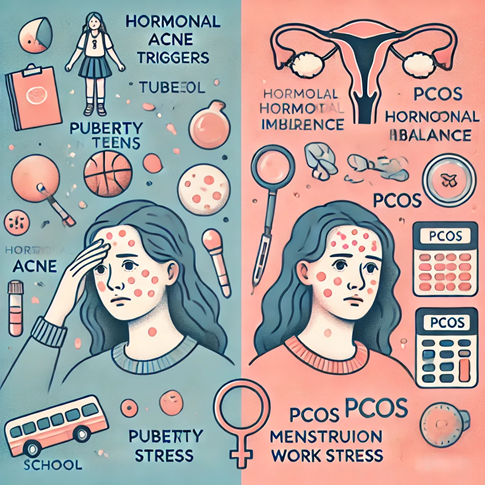
In teens, outbreaks cluster around the jaw and lower cheeks where puberty hormones surge. In adults—especially women—flare‑ups may jump out just before a menstrual period or during high‑stress weeks. A quick fingertip test: press lightly; if the lump feels like a frozen pea under the skin, you are dealing with a cyst.
Keep a three‑month diary of sleep, diet, periods, and breakouts. Even a simple phone note works. When parents help young teens record this, they often spot that late‑night gaming marathons match new cysts. Early flags let you book a derm visit before scarring begins.
The Science of Hormones and Your Skin
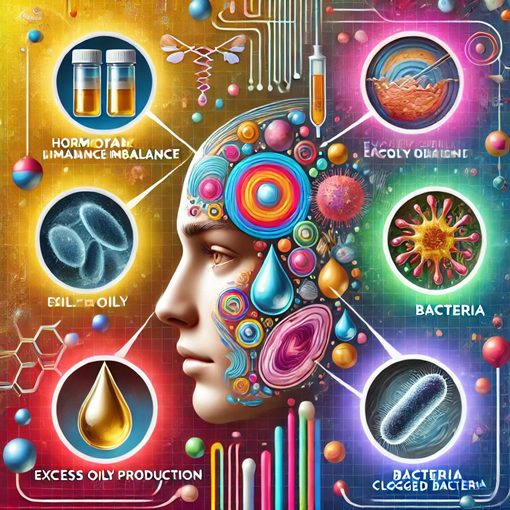
Oil glands respond to a family of hormones called androgens. Boys and girls both make them, but levels spike during puberty, periods, pregnancy, and menopause. Androgens shout, “Produce more sebum!” Extra oil mixes with dead cells, sticks like glue, and blocks the pore. Bacteria inside the follicle gobble this feast and release chemicals that call in the immune system, causing redness and swelling.
Doctors may order blood work if cysts come with extra facial hair or irregular periods. When results show a mismatch, medicines like spironolactone or certain birth‑control pills can level the hormone seesaw.
Genetics and Family Stories: Why Some People Get Severe Breakouts

If one parent battled large, painful cysts, chances are higher you will too. Studies show that mutations in genes controlling skin cell “shedding” and immune response can set the stage. In my practice, siblings sometimes arrive together, both flaring near final‑exam season. Their pores behave a bit like over‑enthusiastic cookie cutters—pushing out thick clumps of keratin that jam the follicle machinery.
Family history also steers how aggressive we get with early treatment. A 14‑year‑old whose mom has deep scars gets a faster referral for isotretinoin than a peer with milder blackheads. This pre‑emptive strike cuts scar risk.
At home, families can compare photo timelines. If a child’s acne looks like Dad’s did at 17, bring those pictures to the dermatologist. Visual records speed the conversation and often convince insurance to cover expensive medications sooner.
Hidden Helpers: How Stress and Lifestyle Sneak In
When you panic before a test or pull an all‑nighter, the body releases cortisol. This hormone can thicken oil, squeeze follicles, and inflame existing cysts. I once counted: after a college basketball tournament, nearly half the team visited me with fresh chin cysts.
Tight helmets, sweaty workout shirts, and heavy makeup also trap heat and oil. Swapping cotton for breathable fabrics cuts cyst counts on the back and shoulders. Encourage young athletes to shower quickly after practice.
Screen breaks, deep‑breathing apps, and eight‑hour sleep blocks sound boring—but data show they slash cortisol spikes. A simple 2‑minutebox‑breathing drill between classes cooled flare‑ups in a small pilot study we ran at our clinic.
The Bigger Picture: Cystic Acne and Underlying Conditions
PCOS, congenital adrenal hyperplasia, and even rare tumors can drive hormone storms. If cystic acne teams up with sudden weight change, hair thinning, or deep voice shifts, call your doctor. Endocrinologists join the team to check insulin resistance and adrenal function.
One teen in my practice had weekly jawline cysts plus dark neck patches (acanthosis nigricans). Lab work showed high insulin. After dietary guidance and metformin, her skin—and blood sugar—calmed down.
Dermatology overlaps with gynecology and endocrinology more than people think. Never feel shy to ask your derm to “phone a friend” for multi‑layered cases.
Doctor’s Toolkit: Prescription Medicines Explained
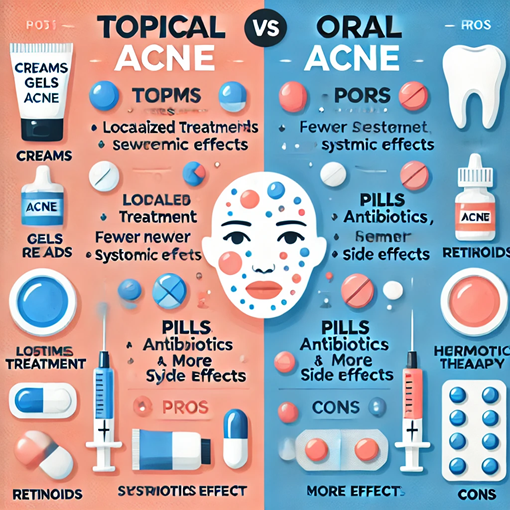
Isotretinoin shrinks oil glands and calms inflammation. Courses last 5‑7 months, with monthly lab checks for liver function and pregnancy tests for girls. Side effects include dry lips and sun sensitivity, but scarring risk drops dramatically.
When isotretinoin is not an option, oral antibiotics like doxycycline tame bacteria and redness. We pair them with topical benzoyl peroxide to slow resistance. After 3‑4 months, we taper to avoid gut imbalances.
Women with hormonal swings may hear about spironolactone. It blocks androgen receptors, lowering oil output. Most notice fewer cysts after two cycles. I remind patients to drink plenty of water, as the drug can raise potassium.
Browse Specials for sample‑size kits that help teens test tolerability without wasting bottles.
In‑Office Procedures: What to Expect at the Dermatologist

A cortisone injection feels like a mosquito bite and shrinks a painful cyst within 48 hours. It is my go‑to for prom‑week emergencies. We never inject the same spot twice in a month to avoid skin dents.
Chemical peels using 30% salicylic or 20% TCA lift stained layers after active acne calms. For deeper pits, fractional lasers drill micro‑columns that spark collagen repair. Kids compare the sound to popcorn—all pops, no pain under numbing cream.
Daily Habits That Protect Your Skin

Use pH‑balanced, fragrance‑free cleansers twice daily. Scrubbing harder will not empty a cyst; it only tears the surrounding skin. Apply non‑comedogenic moisturizer even if you feel oily—dry, cracked skin invites bacteria.
Wash pillowcases twice a week in hot water. For athletes, keep two helmets and rotate while one liner airs out. Swap thick foundation sticks for tinted mineral sunscreen on match days.
Food and Skin: Sorting Facts from Myths
Scientists agree: diet alone does not start cystic acne, but spikes in blood sugar can worsen inflammation. Think of sugary drinks like gas on a small fire. In one summer camp, cabin groups who swapped soda for water had 27% fewer new cysts after six weeks.
Dairy is tricky; skim milk has hormones that may nudge androgens. A two‑month dairy‑free trial won’t hurt and sometimes helps. Replace calcium with fortified soy milk or leafy greens.
Add omega‑3‑rich fish twice a week. These fats calm inflammatory chemicals in skin. Families can try “salmon taco night” as an easy swap.
Curious about gut links?
Our Colosan info explains gentle oxygen‑based cleanses some patients request alongside medical therapy.
Long‑Term Prevention and Monitoring
Schedule skin checks every six months for two years after isotretinoin. Early detection of relapse keeps treatment mild. Parents can set phone calendar alerts labeled “Skin Check” on the child’s birthday and half‑birthday.
Sun protection is vital; cystic skin scars pigment easily. Choose SPF 50 mineral sunscreen labeled “non‑comedogenic.” Reapply after swimming—even clouds let through UV rays that darken scars.
Keep a tiny “rescue kit” in your school bag: hydrocolloid patches, travel cleanser, and a derm’s card. Little tools stop panic from turning into picking.
Frequently Asked Questions
Q 1: Can squeezing a cyst make it heal faster?
A: No. Squeezing pushes infection deeper, lengthens healing time, and greatly raises the risk of scars.
Q 2: How long before isotretinoin starts working?
A: Many patients see fewer new cysts by week 8, but full clearing usually appears after 5–7 months.
Q 3: Will toothpaste or home remedies fix cystic acne?
A: Toothpaste can burn skin. Home hacks rarely reach deep enough to treat cysts; stick with dermatologist‑approved products.
Q 4: Is cystic acne contagious?
A: No. The bacteria involved live naturally on everyone’s skin; cystic acne happens when they get trapped inside blocked pores.
Q 5: Do probiotics help?
A: Some studies suggest certain strains reduce inflammation, but they work best alongside medical treatment, not as a replacement.
Q 6: Can adults over 40 get cystic acne?
A: Yes. Hormone shifts during perimenopause can trigger new cysts even if you escaped teenage acne.
Q 7: Does swimming in a chlorinated pool clear cysts?
A: Chlorine can dry oil briefly, but over‑drying irritates skin and may lead to rebound cysts later.